In March 2020, OMF launched an international, multi-year study across the six OMF supported Collaborative Research Centers (CRC). This was the first study of its kind and the aim is to examine the progression from COVID to Long COVID and the eventual progression to ME/CFS.
In March 2020, OMF brought together its global collaborative network, across 6 research centers in 4 countries, to carry out this global effort in several stages, using an initial $1,000,000 grant donated specifically for this effort. We are actively working to raise additional funding to continue this critical study.
Researchers are testing and analyzing data from individuals from the point of early COVID-19 illness through their recovery or prolonged illness state. This study has an opportunity to reveal what causes one to fully recover versus those at high risk of developing Long COVID and of those, the development of ME/CFS.
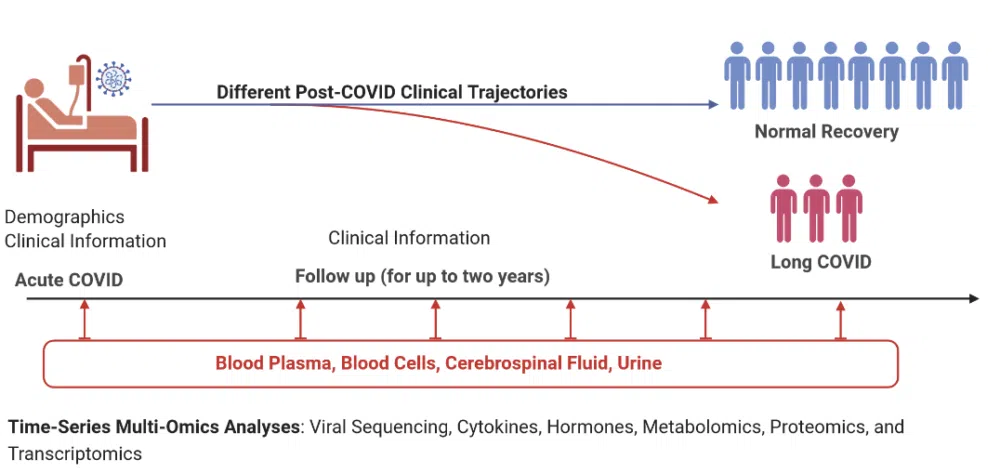
This data is also being compared to the OMF-Funded Post-Viral Complications in Herpes Simplex Encephalopathy (HSE) study data to provide another post-viral contrast. This study design offers the chance to elucidate precise pathological mechanisms of Long COVID, ME/CFS and other post-viral illnesses, identify potential diagnostic biomarkers and validate potential treatment targets for future clinical trials.

Updates from Phase 1
Updates from the Long Covid Clinic at Uppsala
Latest Updates from Montreal
Latest Updates from the Computation Center
Donate your appreciated stock directly to OMFCA and you can receive an immediate income-tax deduction for the fair market value of the securities on the date of transfer (even if you originally paid much less for them).
OMFCA sells your securities and uses the proceeds to support our mission. You also do not pay capital gains tax on the transfer when the stock is sold. Giving appreciated stock can be more beneficial than giving cash. The “cost” of your gift is often less than the deduction you gain by making it. In advance, thank you for making this generous gift.
Gifting of Stock Instructions
Brokerage/Investment Firm: TD Waterhouse
Name on the Account: Open Medicine Foundation Canada
Account Number: 20LRHLA
OMFCA Canadian Revenue Agency (CRA) charity registration #: 74926 5518 RR0001
OMF Canada Registered Address:
Open Medicine Foundation Canada
2987 Baynes Road, Victoria, BC V8N-1Y4
Phone Number: 416-848-0055
Please speak to your personal tax advisor and then call OMFCA at 650-242-8669 to notify us of your donation or with any questions.